WELCOME TO INTEGRATED UNIT (HEMATOLOGY)
-
Introduction
Haematology Unit offers diagnostic investigations in haematology.
-
Sampel Collection and Transportations
- Sample collection
- A correct amount of blood volume as stated on the tube is collected into the appropriate anticoagulant for the test requested.
- To ensure the volume of blood collected is correct, fill the tube to the indicator line.
- The blood should be mixed gently and thoroughly (Please refer to the colour of type of containers, colour, name, anticoagulants used and the test of use in the laboratory)
- All specimens should be sent to the laboratory immediately after collection.
- Delayed transportation of sample may affect the result.
- Sample for urgent cases need to be informed by contacting 04-562 2693.
- Every specimen should be accompanied by details of clinical history and diagnosis in the electronic request or a completely filled request form.
- All samples to be sent to Integrated Unit (Haematology) should use specific containers according to test requested.
TEST CONTAINER TYPE Full Blood Count (FBC)
Blood in EDTA tube
Full Blood Picture (FBP)
Blood in EDTA tube
Routine Coagulation Test (PT / APTT / INR)
Blood in Sodium Citrate tube
D-Dimer
Blood in Sodium Citrate tube
ESR
Blood in EDTA tube
Notes:
- All specimen collection with EDTA, Tri-sodium Citrate and Lithium Heparin tube should be mixed gently and thoroughly for 1 minute by a rotary wrist movement.
- Sample collection
-
Coagulation Test
- Guidelines for specimen collection
- Good specimen collection e.g. clean venepuncture with minimal stasis, not from indwelling catheters or arterial lines, mix well by inverting 5-6 times gently.
- Recommended to use a 21-gauge needle or butterfly. 19 gauge may be used in adults with good veins: 23 gauge may be required for infants.
- Do not use heparin-contaminated venous lines. If unavoidable, flush the lines with crystalloid and discard first few millilitres of blood.
- Correct ratio 1 part of sodium citrate to 9 parts of blood is essential.
- Collect blood to the indicator line on the tube to ensure correct amount of blood collected.
- Send blood to the laboratory immediately.
- The sample ideally tested within 1 hour of blood collection.
- Note down exact time blood is collected.
- Please be noted to sent sample without ice.
- If haematocrit is >0.55, contact laboratory for a tube with adjusted volume of anticoagulant.
- Coagulation screening test
- Where a patient is suspected of having a bleeding disorder, Full Blood Count (FBC) and Coagulation Profile should be performed as a preliminary screen.
- If results are abnormal, or in any case of doubt, the attending clinician should consult Haematologist.
Guidelines for coagulation test
INDICATIONS TEST Warfarin therapy control
PT (Prothrombin Time)
Heparin therapy control
APTT (Activated Partial Thrombin time)
DIC screening
PT, APTT, Fibrinogen level, D-Dimer and platelet count
Liver biopsy
PT (Prothrombin Time), APTT
Pre-operative cases
PT, APTT
- Guidelines for specimen collection
-
Acceptance Criteria for Verbal Requests
- Request should be made less than 4 hours after sample is received.
- Request can only be accepted if the sample is sufficient.
- Requested test is suitable to sample.
- Request should be made by requesting doctor.
-
Outsource Test
List of referral laboratories are as below:
- Jabatan Hematologi, Pusat Pengajian Sains Perubatan, Kampus Kesihatan, Universiti Sains Malaysia, 16150 Kubang Kerian, Kelantan.
- Unit Patologi dan Transfusi Darah, Hospital Kepala Batas, Jalan Bertam 2, 13200 Kepala Batas, Pulau Pinang.
- Makmal Hematologi, Hospital Seberang Jaya, Jalan Tun Hussein Onn, 13700 Seberang Jaya, Pulau Pinang. 04-3827158
- Innoquest Pathology Sdn. Bhd.
- Lablink Medical Laboratory Sdn. Bhd.
-
Turn Around Time (TAT)
CASE TURN AROUND TIME CASE:FBC & FBC-DC
Urgent
Non-urgentTURN AROUND TIME:Within 40 minutes from the time sample is received
Within 160 minutes from the time sample is receivedCASE:FBP
Urgent
Non-urgent
TURN AROUND TIME:Within 2 working days from the time sample is received
Within 5 working days from the time sample is receivedCASE:Routine Coagulation Test (PT / APTT / INR)
Urgent
Non-urgent
TURN AROUND TIME:Within 1 hour from the time sample is received
Within 2 hours from the time sample is receivedCASE:D-Dimer
Urgent
Non-urgent
TURN AROUND TIME:Within 1 hour from the time sample is received
Within 2 hours from the time sample is receivedCASE:ESR
Urgent
Non-urgent
TURN AROUND TIME:Within 1 hour from the time sample is received
Within 2 hours from the time sample is received -
Reference Ranges
-
Normal range of full blood count for adult
-
Normal range of full blood count for children (up to 12 years old)
-
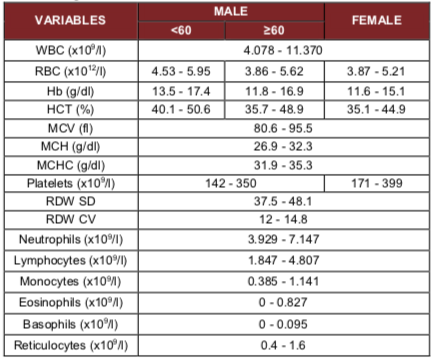 Note: < 60 = Below 60 years old, ≥ 60 = 60 years old and over; Reference: Ambayya A et al., (2014) Haematological Reference Intervals in a Multiethnic Population. PLoS ONE
Note: < 60 = Below 60 years old, ≥ 60 = 60 years old and over; Reference: Ambayya A et al., (2014) Haematological Reference Intervals in a Multiethnic Population. PLoS ONE -
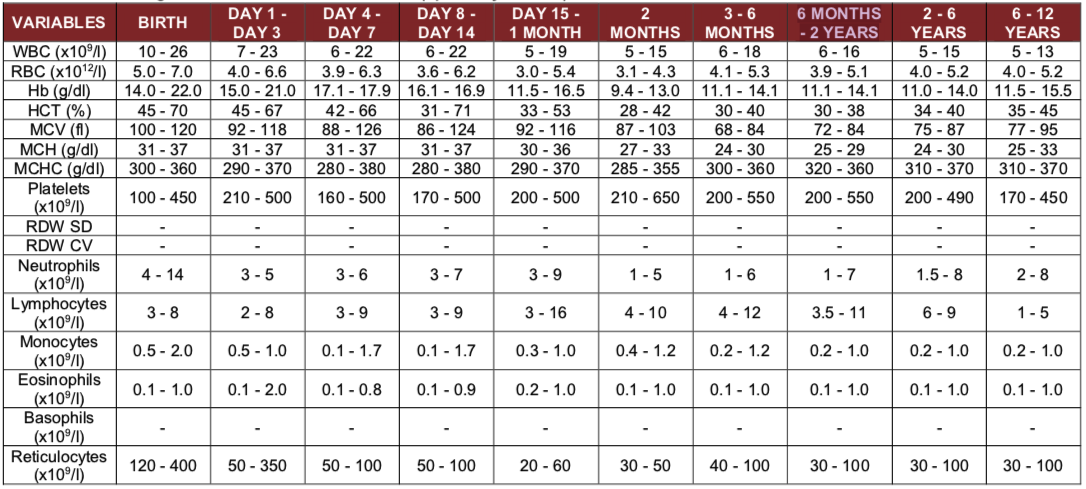 Reference: Dacie and Lewis Practical Haematology, S.M.Lewis, B J Bain and I Bates 12th Edition 2016
Reference: Dacie and Lewis Practical Haematology, S.M.Lewis, B J Bain and I Bates 12th Edition 2016
Coagulation Tests
VARIABLES ANALYZER REAGENT RANGES UNIT PT
INR
APTT
Fibrinogen level
D-dimerSTA-Neoplastine Cl Plus 5
STA-Neoplastine Cl Plus 5
STA-PTT Automate 5
STA-Liquid Fib
STAGO D-Dimer Test12.2 - 14.2
0.97 - 1.18
31.7 - 44.0
2.32 - 4.44
<0.5 / (-)Sec
-
Sec
g/L
ug/mL -
-
Critical Values
Panic value is defined as any result outside the normal ranges to a degree that may pose immediate health risk to patients or require immediate action on behalf of the treating doctors. Laboratory is responsible to immediately NOTIFY doctors of the panic values.
CRITICAL VALUE TEST LOWER CRITICAL LIMIT UPPER CRITICAL LIMIT UNIT Haematology Tests (For Adults)Hb
Hct
Platelet
WBC6
20
20
119
60
1000
50g/dl (adult)
% (adult)
X 109 /L
X 109 /LHaematology Tests (For Paediatrics)Hb
Hct
Platelet
WBC7
20
50
220
40
1000
50g/dl (adult)
% (adult)
X 109 /L
X 109 /LHaematology Tests (For Neonate)Hb
Hct
Platelet
WBC8
25
50
222
70
1000
50g/dl (adult)
% (adult)
X 109 /L
X 109 /LVARIABLES CRITICAL VALUES Coagulation TestsPT
APTT
INR>40 Sec
>100 Sec
>5References:
- Stanford University Medical Center, Hospital and Clinic school of medicine critical values
- www.medicine.uiowa.edu/path_handbook/Appendix/Common/UN_CRIT_LAB_VAL.html critical value for hematology depts.washington.edu/labweb/PatientCare/Clinical/Critical.htm critical value for hematology
- DLMP Critical Values / Critical Results List [CL 041647.004]
- Quick Guide for Notification of Critical Laboratory Results in MOH Hospitals, Institute for Health Systems Research, 2010
- Macking, et al. Guideline on the laboratory aspects of assays used in haemostasis and thrombosis, International Journal of Laboratory Hematology, August 2012
- Stanford University Medical Center, Hospital and Clinic school of medicine critical values





