WELCOME TO TRANSFUSION MEDICINE
-
Introduction
The procurement of blood, the provision of safe and quality blood products and pre-transfusion testing are the main components of the blood bank. Thus, this User Manual serve as guidelines and reference for the clinicians, laboratory personnel and other paramedical staffs to improve the quality of blood transfusion services.
Transfusion Medicine Unit (TMU) located in ADL on the 1st floor of HUSM@Bertam, IPPT. The laboratory provides a 24-hours service. Normal working hours are between 8.10 am to 5.10 pm from Monday to Friday (except public holidays)
-
List of Services, Test and Product
- TMU provides blood donation services and transfusion testing.
- All tests are performed during normal working hours. Only GXM, GSH and Investigation of Transfusion Reaction will be performed after normal working hours.
- An appointment needs to be made for request of special tests.
- Request for special blood products need to be made at least 5 working days in advance.
List of services
SERVICES DETAILS Blood donation
In-house blood donation is opened to staffs and public from 8.30 am till 4.30 pm on working days. Types of donation include whole blood donation and apheresis donation. Apheresis donation is by appointment.
Blood donation campaign
Blood donation campaign is held whenever is necessary inside or outside of TMU.
Stem cell collection
Stem cells are collected via leucapheresis using automated cell separation equipment. The collection is by appointment.
List of tests
TEST ROUTINE SPECIAL Group & Crossmatch (GXM)
✔
Group, Screen and Hold (GSH)
✔
ABO and Rh Grouping
✔
Rhesus Phenotyping
✔
Direct Antiglobulin Test
✔
Antibody Screening
✔
Antibody Identification
✔
Antigen Phenotyping
✔
Investigation of Transfusion Reaction
✔
Isohemagglutinin titre
✔
Antibody titre
✔
Adsorption and Elution Test
✔
Saliva secretor status
✔
Blood products at TMU
TEST ROUTINE SPECIAL DETAILS Blood Components
✔
✗- The blood components available are:
- Whole Blood
- Packed Red Blood Cells
- Random Platelet Concentrate
- Fresh Frozen Plasma
- Cryoprecipitate
Leuco-reduced packed cells
✗
✔
- The leucocyte is reduced to less than 5 x 106 per unit by using a filter. Leucocyte reduced blood is indicated for the following purposes:
- To prevent febrile non-hemolytic transfusion reactions.
- To minimize the risk of transfusion-related CMV transmission.
- To minimize HLA alloimmunization.
Irradiated blood component
✗
✔
The red cell or platelet is irradiated to inactivate lymphocytes to prevent transfusion-associated graft-versus-host disease (TA-GVHD).
-
Forms
Transfusion Medicine Unit provides 5 types of form;
List of forms
FORM PURPOSE It is used to request GXM, GSH and plasma components
It is used to request single immunohematology test other than blood components during offline
It is used to collect blood components from TMU
It is used to request investigation of transfusion reaction
It is used for returning of unused / remnant blood component to the laboratory
-
Container and Sample Management
TEST CONTAINER TRANSPORT STORAGE All
EDTA
Place in biohazard plastic. Sent without ice as soon as possible
In case of delayed transportation, keep the sample in the refrigerator within 2°C - 6°C.
-
Pre-Transfusion
- Consent for Transfusion
- The patient must give written informed consent prior to transfusion.
- The clinician in charge of the patient shall explain to the patient the indication, benefits, risks and alternatives to transfusion therapy, and ensure that the patient understands the issues discussed.
- If for any reason, the patient is unable to personally give consent, a responsible family member of the patient shall be asked to do so. If no such family member is available, or in emergencies when the need for transfusion leaves no time for consent, the decision shall be made by two fully registered medical practitioners. This decision shall be clearly documented.
- Patient Identification
- The phlebotomist shall ensure that the patient is correctly identified by:
- Asking the patient to state their full name and IC number (or use of at least 2 identifiers) in open-ended questions.
- Check the answers given against the information stated on the patient’s identification wristband and/or case notes.
- If it is not possible to identify the patient in the above manner, the phlebotomist shall identify the patient by asking the relative or career to name the patient and then check the answer given against the information stated on the patient’s identification wristband and case notes.
- Patient's Blood Sampling
- The procedure shall be carried out as one process by one person at the bedside.
- Only one patient shall be attended to at any one time till completion.
- The phlebotomist shall clearly and accurately label the blood sample at the patient’s bedside immediately after blood taking.
- Use of HIS pre-printed label is allowed. The ward/clinic should implement a procedure to ensure that patients are correctly identified using the printed labels.
- Information on the label shall include, at the minimum, the patient’s full name, hospital registration number/ identity card number, the date and time of collection and the initial of the phlebotomist.
- Blood Sample and Container for Red Cells Transfusion
- Collect the required amount of blood into the appropriate sample tube as below. Specimen collection with anticoagulant tube should be mixed gently and thoroughly for 1 minute by a rotary wrist movement.
- Infant up to 4 months old
- The sample to be taken from the infant shall be in EDTA pediatric tube (volume is as per stated on the tube container).
- Blood sample in EDTA tube shall be also taken from the mother (volume is as per stated on the tube container).
- Both samples shall be sent to the TMU together under a single request.
- No further sample is required for repeat transfusion of the same set of the paedipack. However, infant’s sample is required for subsequent transfusion if another set of paedipack is going to be issued. For this, crossmatching will be performed using the infant’s sample.
- Infant up to 4 months old
- Older than 4 months old
-
- The sample to be taken shall be in EDTA tube (volume is as per stated on the tube container).
- If a patient requires repeated red cell transfusion, each request for red cells shall be accompanied by a new request form and a new blood sample in EDTA tube (volume is as per stated on the tube container).
- Elective cases
- For elective cases, samples should be sent to the TMU during office hours, at least 24 hours before the blood is required.
- Except for rare blood groups and/or Rh(D) negative where the TMU should be informed at least 5 working days in advance
-
- Collect the required amount of blood into the appropriate sample tube as below. Specimen collection with anticoagulant tube should be mixed gently and thoroughly for 1 minute by a rotary wrist movement.
- Blood Sample and Container (Other than Red Cells) Transfusion
- A new request for blood component other than red cells shall be accompanied by blood sample taken in EDTA tube.
- For a patient who has at least two previous blood grouping records at the TMU, a new blood sample need NOT accompany the request for blood component.
- Borang Permohonan Transfusi Darah
- All requests for blood/blood components must be made using ‘Borang Permohonan Transfusi Darah’.
- The request form should be completely filled and contains relevant patient information.
- Write the name of staff that takes and labels the sample.
- The quantity and the approximate time when the blood and blood component would be required must be stated. Requests for blood to be made available ‘as soon as possible’ should be avoided as this would not assist the blood bank
- personnel in determining priorities.
- The clinician shall ensure that each request form is completed, sign and clearly state his name in block letters or stamped.
- A different request form must be used for different blood components.
- Crossmatched blood will be kept for a further 48 hours.
- Group, Screen and Hold Cases (GSH)
- Tick the appropriate box for a GSH request.
- GSH is a procedure that consists of ABO and RhD grouping, and antibody screening for the patient’s sample.
- It is recommended only for cases where there is a higher chance of requiring a blood transfusion during admission.
- For elective clinical procedures, GSH shall be requested in accordance with the established Maximum Surgical Blood Ordering Schedule (MSBOS).
- Should the patient require transfusion following GSH, blood will be made available on time.
- In case of unexpected antibody was detected, the medical officer in charge will be informed. The laboratory will attempt to supply compatible blood for the patient if required.
- Preferably, the request for GSH is reached at the transfusion laboratory at least 24 hours prior to the operation.
- All GSH request are kept for 72 hours.
- Group and Crossmatch (GXM)
- GXM consists of checking ABO & RhD grouping and antibody screening for the patient’s sample and crossmatching patient and donor unit for compatibility.
- GXM shall be requested for cases with high certainty for transfusion at that time.
- Requests for non-urgent cases such as thalassemia, leukemia, and anemia should be sent preferably before 3.30 pm during normal office hours. This is to ensure that the Medical Laboratory Technologist (MLT) on-call can attend promptly
- and properly to the urgent requests.
- The approximate time when the blood is needed should be stated on the request form.
- Crossmatched blood will be kept for a maximum of 48 hours only. The blood will be automatically canceled on the third day of the request, unless the ward staff or medical officer informs for further reservation.
- Transfusion in Cases of Life-Threatening Bleeding
- Phone call to TMU is required to facilitate the process for Safe O, uncrossmatch or emergency blood request.
- The choice of blood for transfusion in cases of life-threatening bleeding is dependent on the urgency for transfusion and the time available
- Uncrossmatched Group O RhD positive packed red cells (Safe O)
- In Transfusion Medicine Unit, commonly Group O RhD positive packed cells are used as Safe O. Safe O can be used for resuscitation in a dire emergency while waiting for group-specific or crossmatched blood to be available.
- Any decision to use Safe O shall only be made after the clinician has carefully assessed the urgency of the patient’s need for blood. The requesting doctor shall clearly state the reasons for the transfusion in the patient’s records and in the
- request form.
- Tick ‘serta merta tanpa ujian keserasian darah’ box in the request form.
- A pre-transfusion blood sample must be collected from the patient before starting transfusion with ‘Safe O’. Send this sample together with the request form.
- Uncross matched group specific packed cells
- If the blood group of the patient is known, uncrossmatched group specific blood may be given.
- Emergency crossmatch
- If the blood is required urgently (within 30 minutes), tick ‘Segera’ box on the request form.
- The laboratory will issue units of blood that are found to be compatible at immediate spin at room temperature.
- Uncrossmatched Group O RhD positive packed red cells (Safe O)
- For Safe O, uncrossmatch and emergency crossmatch request,
- The laboratory will proceed to completion of the compatibility testing and antibody screening of the units of blood issued, at 37 °C and in the AHG phase.
- If there is any incompatibility detected, it will be immediately informed to the clinician concerned for appropriate action.
- Neonatal Transfusion
- Blood used for neonatal transfusions shall be compatible with the mother’s blood. For that reason, samples from mother and neonate should be obtained.
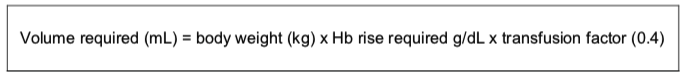
- The volume of blood to be transfused is calculated based on the neonate’s body weight.
- Consent for Transfusion
-
Collection, Transport and Storage of Blood Components
- Issue and collection of blood component
- The ward personnel collecting the blood shall bring ‘Slip Pengambilan Darah /Komponen Darah’ and an appropriate container.
- The laboratory will provide Bed Head Ticket (BHT) sticker to accompany the blood product.
- The laboratory personnel and ward personnel shall verify that the particulars of patient match those of the blood to be issued.
- The laboratory personnel who issued the blood, shall record their name in the request form.
- The person collecting the blood shall record their name, time of collecting and initial in the request form.
- For all wards and private hospitals, which do not have a dedicated blood refrigerator, all cross-matched blood will be kept in the blood bank. Blood must be collected from the blood bank only when it is required for transfusion.
- For wards and private hospitals, which have a dedicated blood refrigerator, blood can be collected for transfusion during normal office hour. However, it is very important that the blood must be stored at 2°C to 6°C in the dedicated blood refrigerator without any undue delay. To maintain the quality of the blood, there must be a quality control program for the dedicated blood refrigerator. The blood bank will assist in the setting up of a quality control program if requested.

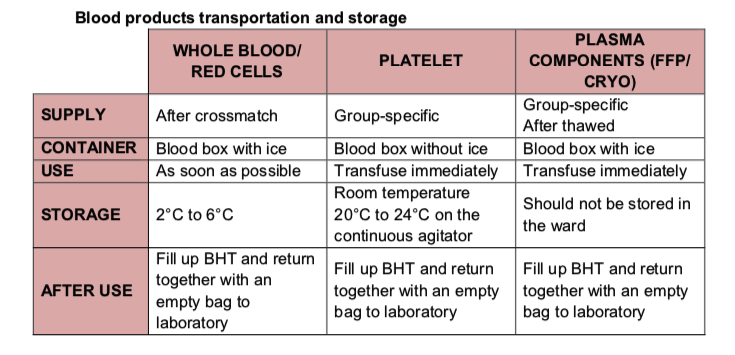
- Transport and Storage
- The ward personnel shall transport the issued blood to the ward or returned blood to the TMU without delay.
- Transportation shall be carried out in an appropriate temperature.
- Issued blood shall be transfused without undue delay. However, in the event where the delay is inevitable, the ward shall maintain the blood at the appropriate temperatures and condition until they are used or returned to the blood bank immediately.
- Whole blood and Packed Cells must not have direct contact with ice packs. There should be a cloth / cardboard in between them to avoid hemolysis.
- Containers for the transportation of platelets must not contain any ice packs. However, for long-distance transportation of platelets in hot and humid conditions or in a non-air-conditioned transport, an ice pack may be put at the bottom of the container in order to sustain an ambient temperature for the viability of the platelets. The platelet must never come into contact with the ice pack.
- Issue and collection of blood component
-
Blood transfusion
- Identification Check Prior to Transfusion
- Each unit / ward shall establish a procedure for carrying out identification checks, to prevent any error occurring at this final stage before transfusion commenced.
- A check shall be conducted to ensure that the patient’s information matches those on the:
- Blood bag label
- Bag Head Ticket / blood compatibility label
- Patient’s identification
- Patient’s blood request form
- Case notes
- The blood shall also be checked to ensure that it has not expired and that it conforms to the following in appearance:
-
- No change in color
- Absence of clots
- No foamy appearance
- No leakage
- In the event of any discrepancy in the identification check of the intended recipient, blood compatibility label, request form and blood component, the laboratory shall be immediately informed. The implicated blood shall be immediately returned to the blood bank for appropriate measures to be taken.
Transfusion of BloodCOMPONENT USE DURATION NOTE Red cells / whole blood
Transfused within 30 minutes of removal from the TMU/ blood refrigerator
The transfusion of each unit shall not exceed 4 hours.
There is significant risk of bacterial contamination if a unit of red cells is kept at room temperature for too long
Platelets
Transfused as soon as it is received from TMU
The transfusion of each pack should not exceed 30 minutes
Platelets should be kept at 20-24° at room temperature and not be refrigerated
Plasma / cryoprecipitate
Transfused as soon as the thawed unit is received
The transfusion should be carried out at a rate that the patient can tolerate
-
- Identification Check Prior to Transfusion
-
Post - transfusion
- Discontinued Transfusion
- Any blood remaining from a discontinued transfusion shall not be used.
- Remnants of blood shall be returned to the TMU immediately together with completed form of ‘Borang Pemulangan Darah Yang Tidak Digunakan’.
- Return of Unused Blood / Blood Component
- The ward shall return all un-transfused blood immediately to laboratory accompanying with completed form of ‘Borang Pemulangan Darah Yang Tidak Digunakan’.
- The ward shall inform the laboratory if any of the un-transfused blood returned to the laboratory has not complied with the storage or transportation temperature.
- Return of Used Blood Bag
- Upon completion of blood transfusion, the ward staff must ensure that the BHT tag / compatibility label attached to each bag of blood component is filled completely and returned to laboratory together with the used blood bag.
- Upon completion of blood transfusion, the ward staff must ensure that the BHT tag / compatibility label attached to each bag of blood component is filled completely and returned to laboratory together with the used blood bag.
- Transfusion Reaction
- If an adverse transfusion reaction is detected or suspected, the transfusion shall be stopped immediately. A doctor shall immediately assess and stabilize the patient. Further management depends on the type and severity of the reaction.
- All transfusion reaction must be investigated. The request must be made using ‘Transfusion Reaction Request Form’.
- To facilitate investigation of an adverse transfusion reaction, follows ‘NOTES’ on the Transfusion Reaction Investigation Request form.
- Preserved the blood bag and tubing set with all attached labels.
- Label specimens as “Post-transfusion”, patient’s name and identifying data.
- For urticarial cases, please send blood bag and transfusion reaction form only.
- Send all investigations sample and request form to TMU immediately.
- Prior to sending the Transfusion Reaction Request Form to TMU, the ward shall keep the transfused blood bag and its transfusion set under appropriate conditions to ensure the integrity and to avoid microbial contamination.
- Discontinued Transfusion
-
Immunohaematology Test Request
Immunohaematology Test Request
- Request for Immunohematology test (other than transfusion request) shall be made only via online, through HIS Care2X.
- The sample to be taken from the infant shall be in EDTA pediatric tube (volume is as per stated on the tube container)
- The sample to be taken for a patient older than 4 months shall be in EDTA tube (volume is as per stated on the tube container).
-
Verbal Request
- Acceptance Criteria for Verbal Requests
- Other than urgent request, the verbal request can be made to add-on blood components, additional testing or to inform cancellation of the test on the previous request.
- For blood component add-on, new hardcopy request form must be sent to TMU.
- Acceptance of verbal request depend on
- Request made less than 24 hours after the sample is received.
- The request can only be accepted if the sample is sufficient.
- The requested test is suitable to sample.
- Request made by / on behalf of the medical officer.
- Order the test / blood component in HIS Care2X
- Acceptance Criteria for Verbal Requests
-
Rejection
Rejection Criteria
- Incomplete relevant information on the request form
- Wrong form
- No name and signature of requesting doctors.
- Information in the request form and sample container is different.
- Wrong sample container
- Mislabeling / incomplete labeling of sample
- Unsatisfactory sample when received, for example, spillages, breakages and etc.
- The sample was taken and labeled by a different person
- Blood hemolyzed
- Blood clotted
- Aged sample (more than 48 hours)
- Insufficient sample
- The test is not available
- Illegible hand-writing
- Double label
- Form has no carbon copy
- No sample or no request form
-
Turn Around Time (TAT)
TEST TURN AROUND TIME TEST:Urgent cases (safe O, uncrossmatch, emergency crossmatch)
TURN AROUND TIME:≤ 30 minutes
TEST:GSH
TURN AROUND TIME:2 hours
TEST:GXM
TURN AROUND TIME:3 hours
TEST:GSH convert to GXM (non-urgent)
TURN AROUND TIME:3 hours
TEST:Request for non-red cells (plasma, cryoprecipitate, platelets)
TURN AROUND TIME:2 hours
TEST:ABO Rh (D) blood group
TURN AROUND TIME:2 hours
TEST:Coomb Test
TURN AROUND TIME:2 hours
TEST:Transfusion Reaction Investigation
TURN AROUND TIME:10 working days
TEST:Other IH Test
TURN AROUND TIME:10 working days
-
Request During Offline
- Request During Offline
- All request shall be made using hardcopy version of ‘Borang Permohonan Transfusi Darah’ or ‘Immunohematology Test Request Form’ accordingly.
- Proceed to request via online (HIS Care2X) once the system is back in operation.







